Cuboid Cobbles Hinder Elite Youth Football Player
Case Report
Description
A 17-year-old elite youth football player was referred to our Academic Center for Evidence based Sports medicine (www.acesamsterdam.nl). The patient was 1.89m in length and weighed 74 kilograms, left-footed and playing on the central midfield position. No specific history to the foot highly relevant to the current diagnosis was noted, apart from the patient presenting with a smaller right foot in length (-1.5 in European size) in comparison to the contralateral side. The patient had developed the current pain on the lateral side of the right foot without a clear traumatic onset and the pain eventually kept him from the pitch and also gave substantial pain on walking in daily life. Prior treatment had consisted of a conservative treatment protocol (immobilization period for 6 weeks) that did not resolve the symptoms.
On physical examination we saw a patient with a slight cavovarus foot. Adequate balance as well as adequate propriocepsis and strength of the musculature of the lower extremity was seen. Walking on his tiptoes was painful (recognizable) on the lateral side of the foot. There was no medial or lateral laxity of the ankle. There was a recognizable pain on palpation of the peroneus longus tendon over the cuboid. Resistance tests of the isolated peroneus longus was also positive for recognizable pain. The peroneus brevis was not painful. The pre-operative patient-reported outcome measures (PROMs) are listed in Table 1.
A peroneus longus tendinopathy was suspected. In order to evaluate both the tendinous component as well as the osseous components (os peroneum, shape of the cuboid, spurs, fragments) it was decided to obtain both an MRI scan (Figures 2, 3, and 4) and CT scan (Figure 5). The CT scan was made additional to the MRI scan due to the fact that the previous MRI scan having been made at a referring center showed a zone of bone marrow edema in the cuboid suggesting the presence of osseous pathology.
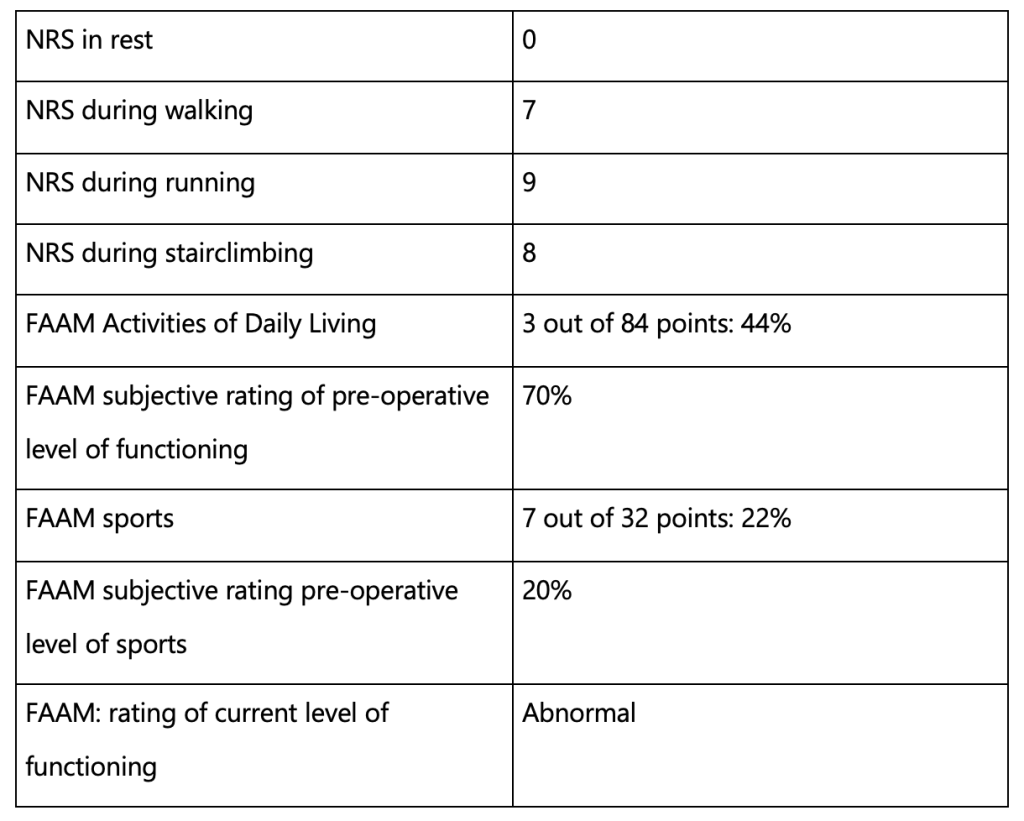
Table 1. Pre-operative patient-reported outcome measures (PROMs)
Diagnosis and Decision-making
The diagnosis was lateral foot pain due to a peroneus longus tendinopathy in the presence of bone spurs in the cuboid groove.
A shared-decision making process with the patient and his family led to a surgical treatment consisting of peroneus longus exploration with an adequate release and reduction of the bone spurs on the cuboidal bone.
Surgical procedure
The patient was operated by the senior author (GK). The patient was placed in a lateral decubitus position for optimal access to the lateral foot. Antibiotic prophylaxis was given with 2g of Cefazoline intravenously. Subsequently the skin was disinfected, and a tourniquet was applied at 250mm Hg on the upper thigh. After draping, a lateral incision was performed directly over the peroneal tendons (Figure 6). The sural nerve was isolated and protected. The peroneus brevis and longus were identified. The brevis was unaffected. The longus was thickened but no major longitudinal ruptures were seen. The tendon was debrided and hypervascularized scar tissue removed from the tendon sheet. Retraction of the tendons was sufficient to expose the bony spurs on the cuboid bone. With small chisels and sharp pliers, the spurs were removed. The wound was flushed, and the wound was closed in layers. Post-operatively, a posterior splint was applied.
Postoperative rehabilitation protocol
The postoperative rehabilitation protocol consisted of a patient-individualized criteria-based structured regime 1. The posterior splint was changed one day post-operatively for a removable cast and the patient was instructed to remain non-weight-bearing for the first 2 weeks post-operatively. The patient was also instructed and advised to perform peroneal activating exercises as well as dorsiflexion and plantarflexion ROM (range of motion) exercises from the first day after surgery for the first 2 weeks under the supervision of a physiotherapist.
Two weeks postoperatively the stitches were removed, and the patient was instructed not to wear the removable cast anymore. A gradual build-up of weight-bearing was allowed as tolerated with the aid of crutches. During week 3 until 6 after surgery, the patient was instructed to continue focusing on the peroneal activating exercises, the ROM exercises and focus on propriocepsis as well as balance training.
At six weeks post-operatively the patient was performing 100% weight-bearing without pain complaints, and he showed an adequate balance as well as propriocepsis thereby completing the postoperative rehabilitation protocol goals of weeks 2 to 6. We instructed the patient and the supervising physiotherapist to focus on a gradual build-up of power and strength focusing especially on the calf musculature and the peroneal musculature, adding exercises for awareness with a special emphasis on symmetrical dorsiflexion with the toes in neutral position as well as mobilization of the plantar fascia. Additionally, the patient was instructed to perform exercises to strengthen the intrinsic muscles of the foot (i.e., foot core). Whenever these goals were targeted and achieved thereafter, a shift towards steadily initiating playful training was allowed with return to running being possible after reaching an adequate ROM as well as a single-leg balance, an adequate walking pattern without joint reaction (swelling/pain), high-quality neuromuscular control and propriocepsis especially containing the peroneus brevis and longus tendon. Gradual return to football with individual training as a start was allowed after fulfilling the previous goal, after which gradual return to group training was allowed whenever the previous goal was achieved in an adequate fashion without tendon reaction.
Outcome and follow-up
The patient was followed-up at 4 years post-operatively. The 4-year follow-up patient-reported outcome measures can be appreciated in Table 2.
10 weeks post-operatively, the patient returned to running.
10 weeks post-operatively, the patient returned to individual football training.
14 weeks post-operatively, the patient returned to football training at group-level in his former team.
18 weeks post-operatively, the patient returned to playing match minutes in his former team.
28 weeks post-operatively, the patient returned to performance being defined as playing 90 minutes at the previous level of football prior to the injury onset.
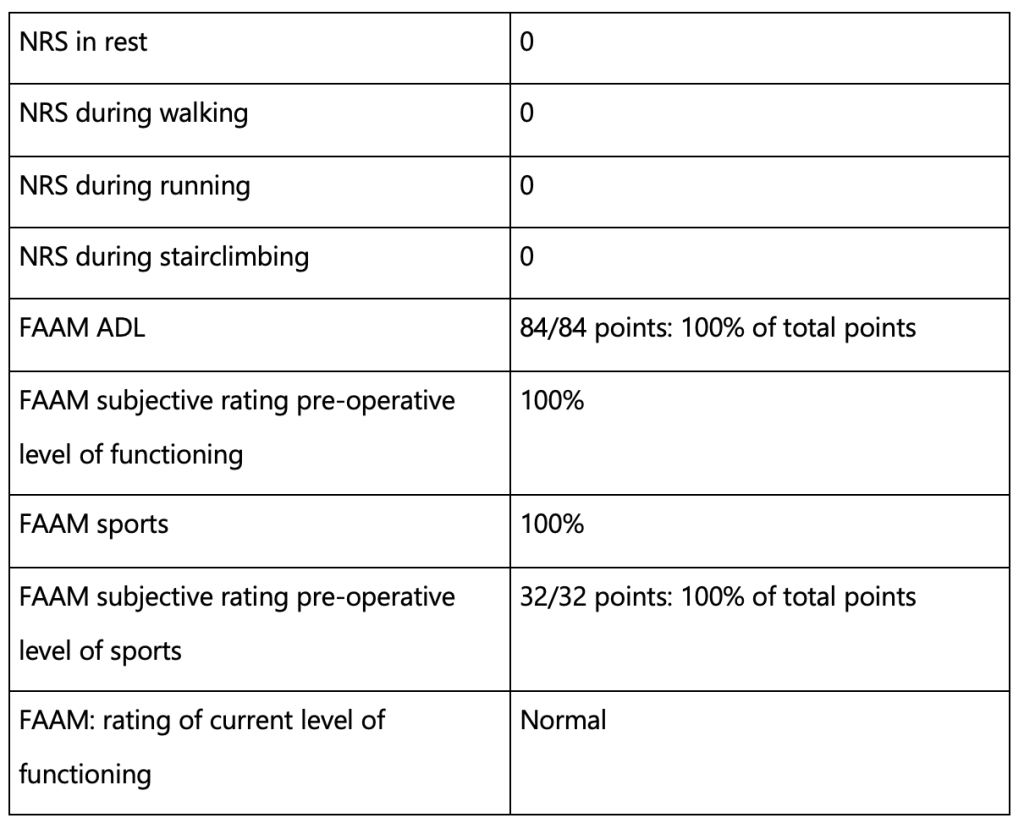
Table 2. Post-operative patient-reported outcome measures (PROMs)
Discussion
In this case report, we describe the diagnostic work-up, treatment and clinical course of an elite youth football player suffering from lateral foot pain due to a peroneus longus tendinopathy due to bony spurs of the cuboid groove. The patient underwent surgical exploration, release, debridement and reduction of the bony spurs after which a strict rehabilitation protocol was initiated. Eventually, he was able to return to performance 1.
Peroneal pathology is a relatively uncommon diagnosis and is associated with long-term sequelae when not managed accurately16. Several anatomic abnormalities may predispose the onset of peroneal tendon pathology5,14. Hardy et al.7 described in their paper the association between quadriceps tendon ruptures due to the presence of patellar spurs. A similar pathophysiological mechanism can be observed in patients with Haglund syndrome 8. When conservative treatment fails to relieve symptoms sufficiently, an endoscopic calcaneoplasty in patients with retrocalcaneal bursitis can yield high patient satisfaction and good long-term functional outcomes12.
Through the presentation of our case, we wish to create awareness to the orthopaedic field that this diagnosis may be present in patients visiting the outpatient department with a peroneal longus tendinopathy not sufficiently responding to an intense conservative treatment protocol. A similar case study has been reported in the literature by Chang et al.4. In their study, the authors aimed to describe the MRI features of cuboid pulley lesions and their associated abnormalities. Other causes of lateral foot pain in athletes consist of POPS (painful os peroneum syndrome) stress fractures of the cuboid or cuboid oedema due to peroneus longus pathology 2,10,11,18.
Conclusion
A 17-year-old elite youth football player was diagnosed with a peroneus longus tendinopathy due to bony spurs in the cuboid groove. A peroneus longus exploration, release and reduction of the cuboidal bone spurs followed by an intensive rehabilitation phase led to a successful return to performance.
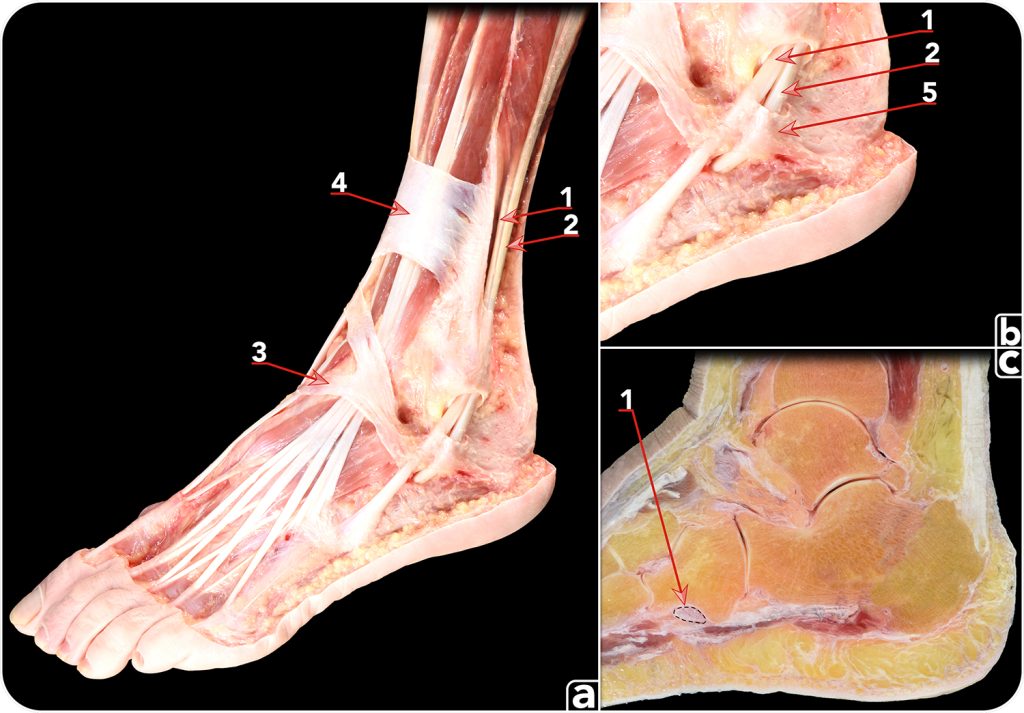
Figure 1: Anatomical dissection (a, b) demonstrating the normal anatomy of the peroneal muscles. 1. Peroneus brevis muscle. 2. Peroneus longus muscle. 3. Inferior extensor retinaculum. 4. Superior extensor retinaculum. 5. Inferior peroneal retinaculum. c) Sagittal cross-section performed at the point where the peroneus longus tendon passes plantar to the cuboid bone. 1. Peroneus longus tendon.
Figure 2: Axial T1-weighted TSE (a) and T2-weighted Spiral (b) MRI Sequence of the right foot. 1. Thickened aspect of the peroneus longus with a bony spur on the lateroplantar side of the cuboid.
Figure 3: Coronal T1-weighted TSE (a) and T2-weighted Spiral (b) MRI Sequence of the right foot. 1. Thickened aspect of the peroneus longus with bony spurs on the lateral and plantar side of the cuboid.
Figure 4: Sagittal T1-weighted TSE (a) and T2-weighted Spiral (b) MRI Sequence of the right foot depicting a thickened aspect of the peroneus longus (1) with a bony spur on the lateroplantar side of the cuboid.
Figure 5: Sagittal (a) and coronal (b) CT scan depicting a thickened aspect of the peroneus longus. 1. Bony spurs on the (latero)plantar side of the cuboid. Normal cuboid anatomy of the contralateral side is shown in (c).
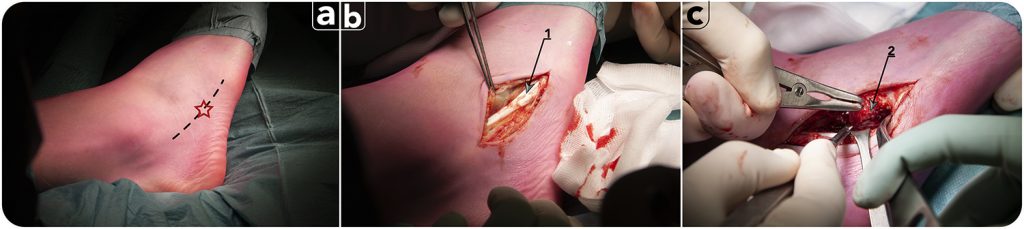
Figure 6: Surgical procedure. a) Incision over the peroneal tendons. Red star indicates the most painful spot over the course of the peroneal longus tendon. b) The incision has been performed and the tendon of peroneus brevis can be seen (1). c) The bony spurs (2) are being removed. Peroneus brevis tendon has been retracted to allow visualization of the cuboid bone.
References
- Ardern CL, Glasgow P, Schneiders A, Witvrouw E, Clarsen B, Cools A, et al. 2016 Consensus statement on return to sport from the First World Congress in Sports Physical Therapy, Bern. Br J Sports Med 2016;50:853-864.
- Beaman DN, Roeser WM, Holmes JR, Saltzman CL. Cuboid stress fractures: a report of two cases. Foot Ankle1993;14:525-528.
- Brandes CB, Smith RW. Characterization of patients with primary peroneus longus tendinopathy: a review of twenty-two cases. Foot Ankle Int 2000;21:462-468.
- Chang MY, Hong SH, Yoo HJ, Choi JY, Chae HD, Moon SJ. MRI of Cuboid Pulley Lesion. AJR Am J Roentgenol 2018;211:867-871.
- Chilvers M, Manoli A, 2nd. The subtle cavus foot and association with ankle instability and lateral foot overload. Foot Ankle Clin 2008;13:315-324, vii.
- Edwards M. The relations of the peroneal tendons to the fibula, calcaneus, and cuboideum. Am J Anat1928;42:213-253.
- Hardy JR, Chimutengwende-Gordon M, Bakar I. Rupture of the quadriceps tendon: an association with a patellar spur. J Bone Joint Surg Br 2005;87:1361-1363.
- Lui TH, Lo CY, Siu YC. Minimally Invasive and Endoscopic Treatment of Haglund Syndrome. Foot Ankle Clin2019;24:515-531.
- Lyman J, Weinhold PS, Almekinders LC. Strain behavior of the distal achilles tendon: implications for insertional achilles tendinopathy. Am J Sports Med 2004;32:457-461.
- Morrison WB, Carrino JA, Schweitzer ME, Sanders TG, Raiken DP, Johnson CE. Subtendinous bone marrow edema patterns on MR images of the ankle: association with symptoms and tendinopathy. AJR Am J Roentgenol 2001;176:1149-1154.
- O’Donnell P, Saifuddin A. Cuboid oedema due to peroneus longus tendinopathy: a report of four cases. Skeletal Radiol 2005;34:381-388.
- Opdam KTM, Zwiers R, Vroemen J, Sierevelt IN, Wiegerinck JI, van Dijk CN. High patient satisfaction and good long-term functional outcome after endoscopic calcaneoplasty in patients with retrocalcaneal bursitis. Knee Surg Sports Traumatol Arthrosc 2021;29:1494-1501.
- Opdam KTM, Zwiers R, Wiegerinck JI, van Dijk CN. Increasing consensus on terminology of Achilles tendon-related disorders. Knee Surg Sports Traumatol Arthrosc 2021;29:2528-2534.
- Saupe N, Mengiardi B, Pfirrmann CW, Vienne P, Seifert B, Zanetti M. Anatomic variants associated with peroneal tendon disorders: MR imaging findings in volunteers with asymptomatic ankles. Radiology2007;242:509-517.
- Syed TA, Perera A. A Proposed Staging Classification for Minimally Invasive Management of Haglund’s Syndrome with Percutaneous and Endoscopic Surgery. Foot Ankle Clin 2016;21:641-664.
- van Dijk PA, Miller D, Calder J, DiGiovanni CW, Kennedy JG, Kerkhoffs GM, et al. The ESSKA-AFAS international consensus statement on peroneal tendon pathologies. Knee Surg Sports Traumatol Arthrosc2018;26:3096-3107.
- van Dijk PAD, Kerkhoffs G, Chiodo C, DiGiovanni CW. Chronic Disorders of the Peroneal Tendons: Current Concepts Review of the Literature. J Am Acad Orthop Surg 2019;27:590-598.
- Yu SM, Dardani M, Yu JS. MRI of isolated cuboid stress fractures in adults. AJR Am J Roentgenol2013;201:1325-1330.